Diabetic Retinopathy
Dedicated to personalized care in a compassionate setting
What Is It?
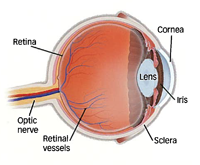 If you have diabetes mellitus, your body does not use and store sugar properly. High blood sugar levels can damage blood vessels in the retina, the nerve layer at the back of the eye that senses light and helps to send images to the brain. The damage to retinal vessels is referred to as diabetic retinopathy.
If you have diabetes mellitus, your body does not use and store sugar properly. High blood sugar levels can damage blood vessels in the retina, the nerve layer at the back of the eye that senses light and helps to send images to the brain. The damage to retinal vessels is referred to as diabetic retinopathy.
Diabetic Retinopathy and Symptoms
Diabetic retinopathy progresses in stages, and early detection can help protect your vision. The first stage — non-proliferative diabetic retinopathy — involves swollen or leaking blood vessels in the retina. You may not immediately notice the symptoms, including blurry vision, dark or empty spaces in your vision and night vision problems.
The second stage — proliferative diabetic retinopathy — occurs when abnormal blood vessels form in the retina. These fragile new blood vessels may bleed, leading to scarring or retinal detachment. Symptoms of PDR include having sudden vision loss, seeing floaters or spots and having difficulty seeing colors. Because this disease develops with few warning signs, those with diabetes should have regular comprehensive eye exams.
Treatment Options
Treatment for diabetic retinopathy depends on your condition’s type and severity. Retina Associates provides several treatment options, including:
- Intravitreal injections: We inject special medications that stop abnormal blood vessel growth and reduce swelling.
- Laser treatment: We use focal/grid photocoagulation to seal leaking blood vessels and slow or stop vision loss.
- Panretinal photocoagulation: This laser treatment reduces abnormal blood vessel growth in advanced stages.
- Vitrectomy surgery: This surgery removes scar tissue and restores vision in severe cases involving bleeding or retinal detachment.
Diabetic Retinopathy Services We Offer
Retina Associates uses state-of-the-art diagnostic tools to detect diabetic retinopathy and monitor its progression. The services offered by our board-certified retina specialists include:
- Dilated eye exams: We look at the back of your eye to detect changes in blood vessels and the retina.
- Optical coherence tomography: This advanced imaging scan displays a cross-section of the retina to detect swelling or fluid.
- Fluorescein angiography: We use dye to highlight blood vessels in the retina and locate leaks and blockages.
- Ongoing monitoring: Our long-term care plans help you manage and monitor diabetic eye health.
When to schedule an examination.
People with diabetes should schedule examinations at least once a year. More frequent medical eye examinations may be necessary after a diagnosis of diabetic retinopathy. Pregnant women with diabetes should schedule an appointment in the first trimester, because retinopathy can progress quickly during pregnancy. If you need to be examined for eyeglasses it is important that your blood sugar be consistently under control for several days when you see your ophthalmologist. Eyeglasses that work well when blood sugar is out of control will not work well when blood sugar is stable. Rapid changes in blood sugar can cause fluctuating vision in both eyes even if retinopathy is not present.
You should have your eyes checked promptly if you have visual changes that: affect either one or both eyes; last more than a few days; are not associated with a change in blood sugar. When you are first diagnosed with diabetes, you should have your eyes checked: within five years of the diagnosis if you 29 years old or younger; within a few months of the diagnosis if are 30 years old and older.
If you have a Non-urgent matter regarding, Appointment Scheduling, Rescheduling, or Cancellation Please Text (520) 617-2852 for appointment requests.
